0117 959 6496
Making Waves in Medical Research
Our grants are helping universities to make life-changing breakthroughs in medical science.
Across our programme areas we are involved in many exciting projects, some of the most novel and interesting come from our medical research stream. This month’s blog will look at some of the research we have funded at universities across the country. We take a keen interest in the work of all Foundation funded PhD students and medical research projects and we would like to share with you a snapshot of the incredible progress currently being made across various fields of medicine.
University of Bristol
As we are based in Bristol, we have a strong relationship with the University of Bristol and have funded various projects there since 2005. We are currently funding PhD research into the effects of aspirin and aspirin alternatives in the treatment of bowel cancer.
Bowel cancer is the 4th most common cancer in the UK and accounts for 10% of mortalities, making it the second most deadly cancer. Worryingly incidence in young adults is increasing and therefore development of new prevention and treatment strategies is crucial.
From 2018 to 2021 we funded Amy Holt’s PhD research. This research found that aspirin was having a profound effect on colorectal cancer (CRC) cell metabolism. Aspirin exposes vulnerabilities in cancer cells which increases the efficacy of treatment to induce cell death. However, the benefits of using aspirin are outweighed by the associated risks of its long-term use such as gastrointestinal bleeding. Amy also looked at a substance similar to aspirin called 5-ASA that has been used for the treatment of ulcerative colitis (UC) for over 30 years. Studies show that 5-ASA is associated with a reduced risk of CRC in patients with UC and importantly, is well-tolerated with less risk of bleeding.
Research by our current PhD student, Ashley Hoskin, is showing that 5-ASA is having a similar effect on cells as that of aspirin in Amy’s research, this is an exciting step-forward and has significant clinical potential. Due to its known safety profile, 5-ASA could be translated to the clinic quickly.
University of Bath
We have been supporting Professor Toby Jenkins at the University of Bath for the past 10 years. His work centres around the development of a revolutionary dressing system for the diagnosis and treatment of paediatric burns wounds.
Across England and Wales, 140,000 patients attend A&E departments with burns every year and on average, 20,000 children require admission to hospital following a burn injury. One of the primary problems in the treatment of burns is bacterial infection, which can delay healing, increase pain, increase the risk of scarring and, in some cases, cause sepsis and death. The changing of burns dressings is a major cause of anxiety, pain and discomfort and also impacts negatively on healing and increases the risk of infection.
The research team at Bath have been developing wound dressings for the past 10 years. Using nanotechnology, they were able to design a gel-based wound dressing which is able to detect clinically significant infection and alert clinicians so they can treat the infection at an early stage. The images below show the change in the dressing overtime as it detects the presence of bacterial toxins.
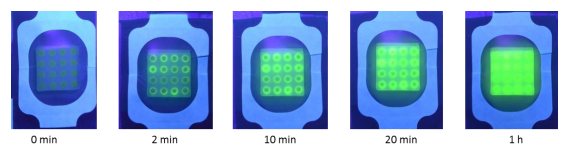
In Spring 2021, they developed a prototype wound dressing material which allows a dressing to be left on a burn wound for longer periods. This ground-breaking invention is currently being patented; it consists of a clear gel (which allows observation of the wound beneath) and a dispersion of polymer capsules dispersed with the gel which encapsulate antimicrobial molecules. This composite hydrogel is activatable via Cold Atmospheric Plasma (CAP): a low temperature jet of electrically excited gas which results in a reduction of swelling and release of an antimicrobial substance to fight infection.
The James Tudor Foundation has recently approved a further three years of funding towards the next stage of this project which aims to answer the following questions:
- Can the composite hydrogel wound dressing in association with CAP be used to control bacterial population in model burn wounds?
- How long can the dressing be left in-situ and still provide microbial control?
- What duration of CAP is needed and on what interval to control model wound infection?
- What is the optimum antimicrobial to use in the dressing?
- How might nurses and patients feel about using such a device in the clinic?
University of Nottingham
We have long standing links with the University of Nottingham and have been funding research into child brain tumours, stem cells and respiratory medicine since 2006. The current research focuses on metastasis (spreading) of tumours. Over one third of patients have evidence of metastasis at diagnosis and sadly the majority of them do not survive.
In 2021, Hannah Jackson completed her PhD investigating the role of exosomes (packages of material released by cells into their environment) in medulloblastoma (the most prevalent malignant paediatric brain tumour). Hannah was able to show that these small packages, which carry messages via bodily fluids, are involved in treatment failure in medulloblastoma. Importantly, Hannah’s data also revealed that as the tumour progressed and became more aggressive the number of exosomes increased.
Work is now ongoing to further understand the reasons for this failure with a view to targeting them in patients and to improve understanding of the drivers of migration in paediatric brain tumours. It is believed that proteins called Rab GTPases (Rabs) play an important role in the creation of exosomes and through a collaboration with a world leading protein expert at the university they aim to broaden their analyses to other brain tumour types and investigate the potential of a Rab targeting approach in brain tumours. Data obtained in studies of medulloblastoma support the hypothesis that Rabs play a fundamental role in driving cell migration in paediatric brain tumours. The aim is now to establish which members of the Rab family are responsible in each tumour type. The team believes that Rabs will serve not only as biomarkers for aggressive types of tumours but also as therapeutic targets. They will therefore either develop a single Rab targeting approach (if the same Rabs drive all paediatric brain tumours) or a targeting approach that targets several types of Rabs. This will drive forward research in this area allowing a more targeted approach to be tested in future clinical trials.
It is fascinating to read about the incredible research being carried out up and down the country to better understand the human body and develop interventions to prevent all sorts of devastating illnesses. If our funding can go a small way towards reducing cancer deaths or reducing wound infection it is money very well spent.